KISII, Kenya, Jun, 10 – Contraception access is crucial to reproductive health and an important facet of any country’s healthcare system.
According to widely available statistics across the developing world, in the past 20 years, contraceptive use has reduced the number of maternal deaths by 40 per cent through the reduction of unintended pregnancies. Following the onset of the COVID-19 pandemic, there are now concerns that the gains made over the years could be reversed following limited access to contraception.
Although health experts have intimated that the complete effects of the pandemic may be felt in years to come, it is still clear that its negative impacts will disproportionately affect developing countries and marginalized communities, exacerbating worldwide sexual and reproductive health and justice inequities.
It is not all doom and gloom however as the global devastation brought about by the pandemic has also presented an opportunity for countries to strengthen their healthcare systems and develop a sustainable solution to the less overt yet alarming crisis of limited contraceptives.
COVID-19 pandemic is already having adverse effects on the supply chain for contraceptive commodities by disrupting the manufacture of key pharmaceutical components of contraceptive methods or the manufacture of the methods themselves such as condoms, and by delaying transportation of contraceptive commodities.
Equipment and staff involved in the provision of sexual and reproductive health services were diverted to fulfill other needs. As some clinics were reportedly shut down, people were reluctant to go to health facilities for sexual and reproductive health services. It was also around the same period when the government restricted movement in a bid to combat the spread of the COVID-19 virus, this expert said affected the access to contraceptives in health facilities.
Access to essential sexual and reproductive health services, and the quality of any care that is provided, declined. Previous public health emergencies have shown that the impact of an epidemic on sexual and reproductive health often goes unrecognized because the effects are often not the direct result of the infection, but instead the indirect consequences of strained health care systems, disruptions in care, and redirected resources.
Esther Bosiboi best encapsulates the challenges Kenyans have gone through in a bid to access contraceptives at the height of the pandemic in the country. The 28-year-old mother of two children from Kisii county said she had to surmount so many challenges including a delicate balancing act of refraining from visiting health care facilities in fear that she may contract the virus.
As a result of the first national lockdown imposed on Kenyans by the government in 2020, Bosiboi says that she was unable to access a contraceptive injection she was using as a family planning method. Consequently, months later she learned that she was expecting a child.
“By then my first-born child was only nine months old, then I realized I was pregnant, something I never planned for. It took me time to accept the siltation but finally, I had to accept and take care of my child, “said Bosibori.

Young adults navigating their way through life also expressed the challenges they underwent during the onset of the pandemic and particularly during the lockdown period. For 23-year-old Belinda Otieno, her decision to abstain from sex since she was unable to access the short-term contraceptive injection she preferred jeopardized her relationship with her partner.
An inability by her partner to also access condoms since they were scarce also worsened her situation.
“Difficulties in accessing contraceptives strained our relationship and despite our best efforts to try and make things work, ultimately, we were forced to go our separate ways, “said the university student.
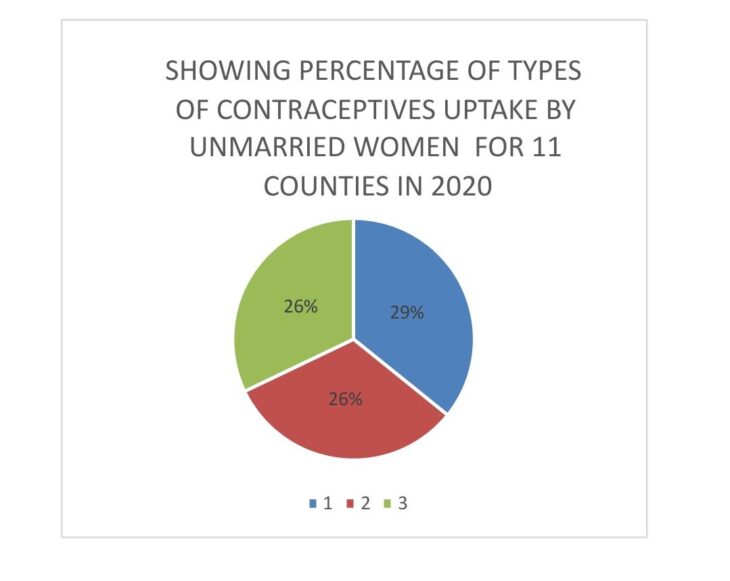
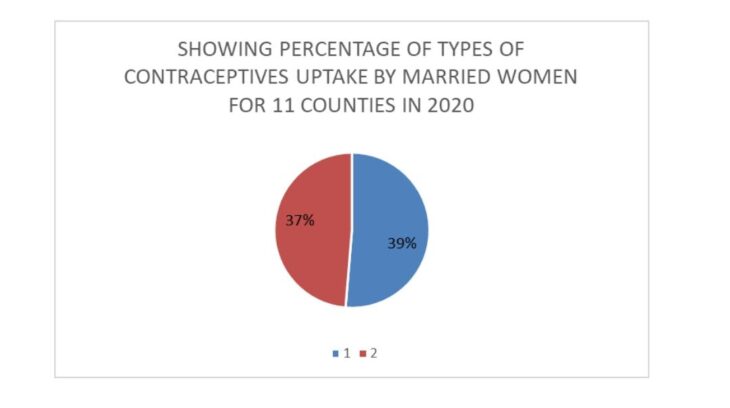
A survey conducted by Performance Monitoring Action between November and December 2021 across 11 counties among them, Nairobi, Kilifi, Nandi, Nyamira, Kiambu, Bungoma, Siaya, Kericho, Kitui, Kakamega, and West Pokot – revealed that unmarried women prefer short-acting methods of contraception while their married counterparts opted for longer-acting methods.
The most popular method for unmarried women was male condoms which represented 29 per cent while injections and implants accounted for 26 per cent.
The married women, on the other hand, preferred injections which accounted for 29 per cent while implants represented 37 per cent.
The Director of Health Services at the Kisii Teaching and Referral Hospital Dr. Geoffrey Otomu says access to contraceptives was low during the height of the COVID-19 pandemic due to containment measures imposed by the government as well as fear of contracting the virus by Kenyans.
“During COVID-19, contraceptives were available at all our health facilities but the uptake of these contraceptives was very low as many feared contracting Coronavirus. Initially, we attempted sensitizing people but their fear of contracting the virus at the time seemed to outweigh their access the contraceptives, “Said Dr. Otomu.
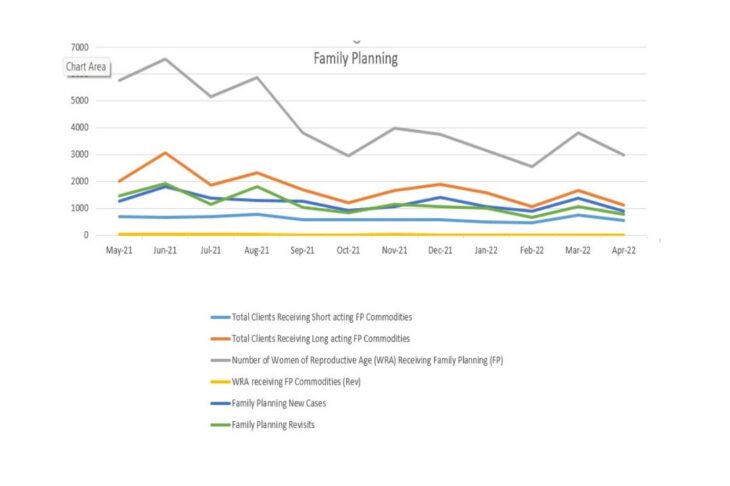
Dr. Otomu now says, there is high uptake of short-term contraceptives such as injections for short periods, and the use of pills on younger and adolescent women compared to older women who go for non-hormonal or long-term injections.
“The usage of contraceptives is high and health care workers have always provided education on the use of these contraceptives thus users are able to make correct choices of the type of contraceptives to use,” he said.
Access of contraceptives is said to have reduced the fertility rate from 6.1 to 3.1 per cent.
With health facilities in Kisii County said to be located at least five kilometers from each other, access to contraception is said to have been simplified amongst women while men only turn out for condoms. Worth noting is that no case has ever been recorded on sterilization contraceptives.
Principal Secretary of Health Susan Mochache said COVID-19 put a strain on the country’s health care system paralyzing various services which were experienced and documented as people kept away from hospitals including those who needed contraceptives, TB, and ARVs services.
“COVID-19 was a global problem and there is no country whose health systems were not affected either from the stress of managing the pandemic or fear of people coming to hospitals to get these services,” said Mochache who further said, “When protocols were in place people feared getting out to go to hospital and also misunderstanding on COVID-19 paralyzed access of health services including access to Contraceptives.”
The ministry of health has now revealed that with a sense of normalcy slowly creeping back to the country women can now access family planning services in various hospitals nationwide.
Counseling psychologist David Omandi said the supply chain of these contraceptives was cut off and no clear guidelines were given on public health as nations concentrated on the fight against the spread of COVID-19.
According to Omandi, about 1.4 per cent of people had unplanned pregnancies leading to a high rate of abortions and unsafe abortions.
“Poor access of contraceptives led to an increase of birth rates across the globe, sexual violence among couples leading to psychological torture,” says Omandi.
Poor access to contraceptives also led to stress and depression among women and girls. Equally, the lack of adequate social workers and counselors is said to have contributed to untold suffering among scores of people.
Edinah Kangwana a human rights activist in Kisii County says at the height of the pandemic, there were no clear guidelines on reproductive health, and addressing the gap in contraceptive use proved difficult.
“I personally went to the villages to preach this gospel. I used Nyumba kumi leadership, the village elders, the chiefs, and the clergy to reach our women at the grassroots. However our efforts provide futile as many feared coming out in order to receive these services,” she said.
Through her social outreach programme, however, he managed to incorporate reproductive health officers across health facilities and managed to organize sessions with individuals in order to boost their confidence. A hotline number availed to women also helped them seek help or clarification on health concerns they had.
“In the session, we talked broadly on sexual and reproductive health, economic empowerment, women and leadership, mental health, Gender-based violence and the issue with the then high numbers of teenage pregnancy and the role mothers could play to curb the disaster,” said Kangwana.
The programme was also able to provide women and girls with menstrual hygiene products.
Want to send us a story? Contact Shahidi News Tel: +254115512797 (Mobile & WhatsApp)


